I have a general question regarding how veterinarians administer and dose the radioiodine ( I-131) as treatment for hyperthyroid cats. Although I have had a number of my hyperthyroid patients treated successfully with radioiodine, I do not know how one administers and doses it. A little explanation would be appreciated.
My Response:
We've been giving the radioiodine subcutaneously since 1986. Prior to that, we initially tried the oral route, but that meant handling radioactive capsules (and hoping the cat's wouldn't chew them) or stomach tubing the cats (and hoping the cats wouldn't vomit). In human patients, they generally put the radioiodine solution into a juice drink to cover up the 'iodine" taste and the people just drink the solution. Obviously, that wouldn't work in cats.
 From around 1980 to 1986 we gave all of the doses IV, which worked fine. However, that meant that two people always needed to be exposed when the dose is administered and the cat needed to have a catheter placed for the injection. The IV administration worked well, but occasionally, I saw anaphylactoid reactions (rather terrifying!) upon treatment. Obviously, there is something in the solution that that cats don't like when the drug is given more than once intravenously.
From around 1980 to 1986 we gave all of the doses IV, which worked fine. However, that meant that two people always needed to be exposed when the dose is administered and the cat needed to have a catheter placed for the injection. The IV administration worked well, but occasionally, I saw anaphylactoid reactions (rather terrifying!) upon treatment. Obviously, there is something in the solution that that cats don't like when the drug is given more than once intravenously.
Today I still administered the radioiodine to all of my hyperthyroid cats by the subcutaneous route. In many of these cats, I can perform the treatment by myself, thereby not exposing another member of my staff to the full dose of radiation that is contained in the syringe. I have NEVER seen an anaphylactoid reaction when the radioiodine solution is given subcutaneously.
As far as dosing goes, I really do believe that facilities that use a 'fixed dose' are overdosing most of the cats, and under-dosing others.
I give a range of doses from 2-10 mCi to cats with benign adenoma (adenomatous hyperplasia). This method of dose determination is somewhat more complicated, and is based on the following factors:
* Clinical severity of hyperthyroidism
* Size of thyroid tumor(s) on palpation
* Result of thyroid scintigraphy (thyroid scanning)
* Age of the cat
* Known concurrent diseases
Cats with thyroid carcinoma generally require much larger radioiodine doses, generally in amounts of around 30 mCi but sometimes even more. These cats generally have larger thyroid masses, generally invading soft tissue and extending into the thoracic cavity.

Hyperthyroid cat with thyroid carcinoma (on left) demonstrating the massive, multinodular tumor, invading and extending into the thoracic cavity. The horizontal line is the region of the thoracic inlet.
My goal of therapy is to 'cure' the hyperthyroid state without causing hypothyroidism. Many treatment facilities boast about the fact that they can cure 98% of hyperthyroid cats. Well, that's easy; anyone can order a big dose for all hyperthyroid cats and cure them, but many will become hypothyroid. I agree it's more difficult to titrate the doses because one has to think about the whole cat and what we are doing, but I do believe it's so very important. That's where this whole treatment issue become more tricky.
It's becoming increasing clear that both hyperthyroidism and hypothyroidism are bad for the kidneys, so that last thing we want to do is cure the hyperthyroidism but create iatrogenic hypothyroidism. And that is especially true if the owners cannot give oral medication or if the cat already has mild renal disease.
Źródło: endocrinevet.blogspot.com
Our pharmacist is telling me that determir insulin (Levemir) expires after 30 days. He claims that this is because of the risk of contamination.
At $112 a bottle, this short expiration date would make detemir cost prohibitive for my clients. Is detemir insulin actually stable for longer periods if kept refrigerated, as has been found with glargine insulin (Lantus)?
My Response:

Glargine is marketed for human use with a 28-day shelf-life at room temperature after opening. Similarly, detemir is marketed with a 6-week shelf-life at room temperature after opening of the vial.
The recommended shelf-lives for both detemir and glargine are relatively short, not because of lack of efficacy, but because of the increased risk of bacterial contamination with these multiple-use,
injectable medication vials. The FDA believes that the insulin vials may have a high probability of becoming contaminated with microbes by the daily multiple punctures needed to withdraw medication when used past the insulin's expiration date.
For veterinary use, we generally recommend that both insulins be kept refrigerated, although theantimicrobial preservative in these insulins may actually be more effective at room temperature. Owners of diabetic cat or dogs use refrigerated glargine or detemir routinely for up to 6 months without evidence of problems occurring. The insulin should be discarded immediately, however, if any cloudiness or discoloration is noted.
This issue with bacterial contamination seems to be extremely rare. Pet owners are much more likely to accidentally drop and break the vial, than to have to throw it away because it develops discoloration.
Źródło: endocrinevet.blogspot.com
Her serum parathyroid hormone (PTH) concentration is high (32.3, normal 3.0-17.0), ionized calcium is high (1.92, normal 1.25-1.45), and the parathyroid hormone-related polypeptide (PTHrp) is negative (0.0, normal 0.0-1.0). No gross evidence of perianal masses are seen including on rectal exam, and no lymph node enlargement can be palpated.
Will this be enough evidence to say that this dog definitely has primary hyperparathyroidism? Or should we do more to rule out other malignancy as the cause of hypercalcemia in this dog?
My Response:
Yes, it certainly does appear that your dog has primary hyperparathyroidism. I'd recommend chest radiographs and abdominal ultrasound to complete the workup, but they will likely be normal.
If you can do a parathyroid ultrasound, that would be recommended especially if surgical parathyroidectomy is planned.
Next question:
Sorry to be a bother, but no chance that this dog couldn't have hypercalcemia of malignancy?
How about renal renal secondary hyperparathyroidism or nutritional secondary hyperparathyroidism?
My Response:
Hypercalcemia of malignancy is possible but extremely unlikely in this dog. While hypercalcemia of malignancy does not always produce high levels of PTH-rp, the PTH concentration should be low in that situation, not high as is the case in your dog.
Unless the dog is eating some bizarre diet, we can rule out nutritional disease in a dog of this age, and I assume the dog is not in renal failure at this time, which largely eliminates that consideration. So primary hyperparathyroid disease remains the most likely by far.
Źródło: endocrinevet.blogspot.com
Treatment with arginine vasopressin (antidiuretic hormone of humans, dogs, and cats) or its analogues restores medullary hypertonicity and a normal urinary concentrating ability in animals with central diabetes insipidus. Historically, ADH tannate in oil, an extract of arginine vasopressin prepared from bovine and porcine pituitary glands, was administered every 2 to 3 days as needed to control polyuria and polydipsia. Because this product is no longer available, desmopressin acetate, a synthetic analogue of arginine vasopressin with prolonged and enhanced antidiuretic activity, has become the drug of choice for the treatment of central diabetes insipidus in dogs and cats.
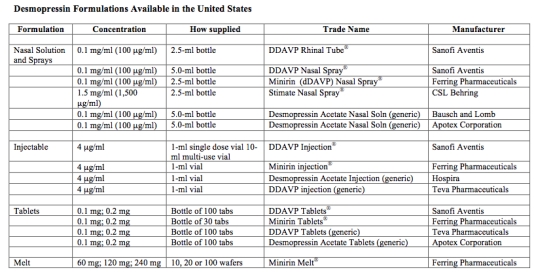
DESMOPRESSIN PREPARATIONS
Desmopressin acetate is available in preparations for intranasal, parenteral (injectable), or oral administration (see Table below).
Nasal sprays or solutions of desmopressin
The nasal formulations are supplied with 2 different delivery systems: either a spray pump or a rhinal tube delivery system (see Table below), in which the desmopressin is “sprayed” or “blown” into the nose, respectively. Obviously, most dogs or cats will not tolerate either of these intranasal delivery methods. Drops placed in the conjunctival sac provide a more suitable alternative for animals.
With the rhinal tube delivery formulation (DDAVP Rhinal Tube®, Sanofi Aventis), the desmopressin is packaged with a small, calibrated plastic catheter so that exact amounts of the drug can be measured and administered. The calibrated rhinal tube has four graduation marks that measure amounts of 0.05 ml, 0.1 ml, 0.1 ml, and 0.2 ml and thereby can deliver doses of 5 to 20 µg of desmopressin). Although this system allows for accurate dosing, it is awkward to use. In addition, because this rhinal tube delivery system is not available as a generic product, this formulation is quite expensive.
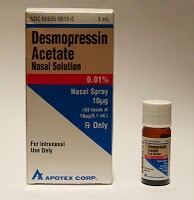
 The most common intranasal formulations of desmopressin are marketed as nasal sprays or solutions equipped with compression pump that delivers 10 µg of drug with each spray. For use in dogs and cats, this spray bottle should be opened (a plier may be neccessary to break the seal) and the desmopressin solution transferred to a sterile vial; this dispensing vial then allows one to place the desmopressin drops within the animal’s conjunctival sac.
The most common intranasal formulations of desmopressin are marketed as nasal sprays or solutions equipped with compression pump that delivers 10 µg of drug with each spray. For use in dogs and cats, this spray bottle should be opened (a plier may be neccessary to break the seal) and the desmopressin solution transferred to a sterile vial; this dispensing vial then allows one to place the desmopressin drops within the animal’s conjunctival sac.
 These intranasal preparations of desmopressin are generally supplied as a concentration of 100 µg/ml; depending on the size of the drop, one drop of nasal solution corresponds to 1.5 to 4 µg of desmopressin. One highly concentrated nasal solution (1.5 mg/ml) is marketed for use in hemophilia (see Table below), but it should not be used to treat animals with diabetes insipidus because of the strong likelihood of overdosage.
These intranasal preparations of desmopressin are generally supplied as a concentration of 100 µg/ml; depending on the size of the drop, one drop of nasal solution corresponds to 1.5 to 4 µg of desmopressin. One highly concentrated nasal solution (1.5 mg/ml) is marketed for use in hemophilia (see Table below), but it should not be used to treat animals with diabetes insipidus because of the strong likelihood of overdosage.
In most cats and smaller dogs, 1 to 2 drops of the intranasal preparation administered once or twice daily are sufficient to control polyuria and polydipsia. Larger dogs may require up to 4 to 5 drops twice daily. Use of a tuberculin or insulin syringe allows for more accurate dosing. Application of desmopressin into the conjunctival sac may cause local irritation, as the solution is acidic. Some animals may object to the daily eye drops, making this route of administration ineffective.
Oral desmopressin tablets
The oral preparation of desmopressin is available both as a sublingual dissolve melt tablet (not suitable for treating cats) and as 0.1 mg and 0.2 mg tablets. Each 0.1 mg (100 µg) tablet is roughly comparable to 5-10 µg (1-2 large drops) of the nasal solution (see Table below).
 The tablet form of desmopressin is a more cost-prohibitive alternative compared with the conjunctival or subcutaneous routes of administration. The cost of daily oral desmopressin in animals is roughly 2.5-times that of the cost of conjunctival drops, and roughly 6 times the cost of subcutaneous injections of desmopressin. For some pet owners, however, the use of a tablet form may prove to be a more convenient, or the only possible route of administration that is possible.
The tablet form of desmopressin is a more cost-prohibitive alternative compared with the conjunctival or subcutaneous routes of administration. The cost of daily oral desmopressin in animals is roughly 2.5-times that of the cost of conjunctival drops, and roughly 6 times the cost of subcutaneous injections of desmopressin. For some pet owners, however, the use of a tablet form may prove to be a more convenient, or the only possible route of administration that is possible.
Injectable desmopressin solutions for SC or IV use
 An injectable sterile solution of desmopressin acetate (4 µg/ml) marketed for intravenous use is available (see Table) and can be used in animals with diabetes insipidus. However, the cost of the injectable desmopressin is approximately 7 to 15 times higher per µg than the intranasal preparation, making this formulation cost-prohibitive for use in most dogs and cats.
An injectable sterile solution of desmopressin acetate (4 µg/ml) marketed for intravenous use is available (see Table) and can be used in animals with diabetes insipidus. However, the cost of the injectable desmopressin is approximately 7 to 15 times higher per µg than the intranasal preparation, making this formulation cost-prohibitive for use in most dogs and cats.
To circumvent this cost iss
ue, the intranasal form of desmopressin – although not designed for parenteral use – can be given subcutaneously to cats with excellent results. Because the nasal forms of desmopressin are not considered to be sterile, however, it is best to first sterilize the product by passing the nasal solution through a 0.2 micron bacteriostatic syringe filter. Clinically the nasal and injectable preparations of desmopressin induce indistinguishable responses when administered subcutaneously.
To make dosing easier, the desmopressin is best administered with an U-100 low-dose insulin syringe. The solution can be diluted in sterile physiologic saline to make dosing easier.
The subcutaneous route of desmopressin administration has many advantages over the other routes of administration. These advantages include the following:
* First, drug appears to be most effective when administered via the subcutaneous route.
* Second, the duration of action is longer after subcutaneous injection than when administered orally or via the conjunctival sac.
* Third, because of the smaller subcutaneous doses required to control signs (about 15% and 40% of the oral and conjunctival doses, respectively), the cost of treatment is greatly reduced.
* Fourth, many cats seem to prefer long-term subcutaneous injections to the chronic use of eye drops or oral medication.
Company Web sites for more information:
- Sanofi Aventis
- Ferring Pharmaceuticals
- CSL Behring
- Bausch and Lomb
- Hospira
- Teva Pharmaceuticals
- Apotex Corporation
Desmopressin acetate is also available generically (many companies) and may also be known by the following synonyms and internationally registered trade names:
Concentraid®, D-Void®, Defirin®, Desmogalen®, Desmospray®, Desmotabs®, Emosint®, Minurin®, Nocutil®, Octim®, Octostim®, or Presinex® Źródło: endocrinevet.blogspot.com
Źródło: endocrinevet.blogspot.com
Once a diagnosis of diabetes insipidus has been confirmed, the next step to start replacement treatment with desmopressin.
Initial treatment with desmopressin
 Recommended initial doses of desmopressin vary depending on the route it is being administered. In most cats and smaller dogs, 1 to 2 drops of the intranasal preparation administered once or twice daily are sufficient to control polyuria and polydipsia (see Table below). Larger dogs may require up to 4 to 5 drops twice daily. Use of a tuberculin or insulin syringe allows for more accurate dosing. Application of desmopressin into the conjunctival sac may cause local irritation, as the solution is acidic. Some animals may object to the daily eye drops, making this route of administration ineffective.
Recommended initial doses of desmopressin vary depending on the route it is being administered. In most cats and smaller dogs, 1 to 2 drops of the intranasal preparation administered once or twice daily are sufficient to control polyuria and polydipsia (see Table below). Larger dogs may require up to 4 to 5 drops twice daily. Use of a tuberculin or insulin syringe allows for more accurate dosing. Application of desmopressin into the conjunctival sac may cause local irritation, as the solution is acidic. Some animals may object to the daily eye drops, making this route of administration ineffective.
With the subcutaneous route of administration, the initial recommended dose is 1.0 to 5.0 µg once or twice daily, depending on the size of the animals. If the nasal solution (100 µg /ml) were used for this purpose, one would inject only 0.01 to 0.05 ml (or 1 to 5 U with a U-100 insulin syringe). With the oral tablets, a starting dose of 0.05 mg to 0.2 mg (50 to 100 µg) once or twice daily is initiated.
Desmopressin dose adjustments
In dogs and cats with central diabetes insipidus, daily administration of desmopressin may completely eliminate polyuria and polydipsia. However, because of individual differences in absorption and metabolism, the dose required to achieve complete, around-the-clock control varies from patient to patient. The maximal effect of desmopressin occurs from 2 to 8 hours after administration, and the duration of action varies form 8 to 24 hours. Larger doses of the drug appear to both increase its antidiuretic effects and prolong its duration of action; however, expense can become a limiting factor for some owners.
No matter what route of administration is used, the daily dose should be gradually adjusted as needed to control signs of polydipsia and polyuria. The morning and evening doses can be adjusted separately if needed.
Adverse effects of desmopressin
Desmopressin is relatively safe for use in animals with central diabetes insipidus. Adverse effects of desmopressin are uncommon, but overdosage can lead to fluid retention, hyponatremia, and decreased plasma osmolality. Although extremely rare, fluid intoxication associated with desmopressin overdosage can lead to CNS disturbances including depression, increased salivation, vomiting, ataxia, muscle tremors, coma and convulsions. In such instances, furosemide can be given to induce diuresis.
To avoid the potential problem of overdosage, it is recommended that animals not be allowed free access to water immediately after each dose of desmopressin, especially if severe polydipsia and polyuria have redeveloped. Without such short-term (1 to 2 hours) water restriction, the cat many consume excessive amounts of water that cannot be subsequently excreted, as the desmopressin is absorbed and has its peak antidiuretic effects on the renal tubules.
Cost of desmopressin
The principle drawback with the use of any of the desmopressin preparations in the treatment of central diabetes insipidus is the drug’s considerable expense. The oral route of administration is the most expensive, while the subcutaneous route of administration (using the sterilized nasal solutions) is generally the most cost-effective.

Źródło: endocrinevet.blogspot.com
I have a 12 year old male neutered Maine coon cat that has a free T4 (measured by equilibrium dialysis) of 57.9 nmol/L (normal is up to 50 nmol/L). The cat has stable weight and no real signs of hyperthyroidism. Other blood is good. Just wondering how we should follow up. I am contemplating re-assessing in a month or two? What is the correct approach to this case?
Thanks in advance.
My Response:
Monitor the cat's body weight, heart rate, thyroid size, and serum total T4 concentrations every 2-3 months.
Hyperthyroidism is a clinical diagnosis. The finding of a high serum free T4 value means nothing unless you have clinical signs, or a palpable thyroid nodule, or both.
Źródło: endocrinevet.blogspot.com
I don't know if I should even ask this but a situation in my family has me curious. My sister-in-law was diagnosed with pituitary-dependant Addison's disease over five years ago. She has been treated since that time with florinef and prednisone and has been doing well. Recently she had a recheck and an ACTH stimulation test while on treatment and she had a resting cortisol around 10 µg/dl and post around 20 µg/dl.
Now she's being weaned off of treatment and told her pituitary and adrenals are fine. I've never done an ACTH stimulation test on an animal I'm treating for Addison's disease after it's diagnosed and was wondering about the rational for doing that. Is human Addison's disease curable? Is there something completely different in human Addison's from the canine disease, or am I just missing something?
If anyone has an opinion and would like to share I'd appreciate it. Curiosity is getting the best of me. Thank you.
My Response:
It sounds to me as if they didn't believe the diagnosis of Addison's disease so they repeated the ACTH stimulation test. Addison's disease doesn't resolve once it develops (in either dogs or humans), and there is no such thing as "pituitary-dependent" Addison's disease.
On a brighter note, its's great news that your sister-in-law is normal!
Couldn't you theoretically get glucocorticoid deficiency from lack of production of ACTH? (Kind of like a central diabetes insipidus dog having a central lesion?)
My Response:
Absolutely. But pituitary ACTH deficiency is "secondary" hypoadrenocorticism, not Addison's disease.
Sorry to be such a stickler about terminology, but when Sir Thomas Addison described the disease that now uses his name, all of the patients had "primary" hypoadrenocorticism with complete destruction of both adrenal cortices.Therefore, the term Addison disease should be restricted to those patients with the primary form of the disorder (ie, those that have both glucocorticoid and mineralocorticoid deficiency).
There is no such disease as pituitary Addison's disease. Why? Because, like we all know, pituitary ACTH deficiency can not cause destruction of the adrenal gland or lead to mineralocorticoid deficiency. ACTH deficiency would only cause cortisol deficiency.
When we use the term Addison's so loosely, it becomes very confusing. It really would be best to avoid the use of the term completely. But we know that will never happen!
Źródło: endocrinevet.blogspot.com
This patient is a 5.5-year-old male neutered Westie that presents with the main complaints of polyuria and polydipsia (PU/PD). The results of a CBC and serum chemistry panal were normal. Strangely, however, the dog has glucosuria with no hyperglycemia. We have run multiple samples on different days of both blood and urine, all showing positive glucosuria but normoglycemia.
I submitted a urine cortisol:creatinine ratio (UCCR)to screen for Cushing's syndrome. It was not the ideal, home-caught, first in AM urine sample. It was free catch urine sample collected here at the clinic. Results show a UCCR ratio of 115. But the urine cortisol is 8.5 µg/dl (normal for Idexx laboratories reference range) and the creatinine is 23.1 mg/dl (low for the reference range). So, am I correct to interpret that the ratio is high because the creatinine is low and not because the cortisol is high? Can Cushing's syndrome be ruled out, or should I proceed to further Cushing's diagnostics?
My Response:
We do the UCC-ratio to correct for increased/decreased filtration and we therefore ought to look at the ratio, not the individual results. Therefore we cannot rule out Cushing's syndrome based on this result. You could, however, repeat measurements on a few home collected, morning samples. It is interesting that the serum alkaline phosphatase is normal in this, which, although still possible, makes hyperdrenocorticism less likely. It still is an important differential though. You could also run a fructosamine to check for chronic relative hyperglycemia.
Źródło: endocrinevet.blogspot.com
Agatha is an 11-year-old F/S DSH first seen 3 months ago. The owners complained that she had beeen moping around for the past week and was more "clingy" than normal. She had vomited twice and urinated outside of the box on a few ocassions. My physical examination at that time was completely normal. Her heart rate was 168 bpm, there were no palpable thyroid nodules, and her weight was 11.3 pounds.
I saw the cat again last week, with the new complaint of sounding hoarse for 3 weeks. The cat was also eating and drinking less, and she was lethargy and less active. My physical examination revealed that her body weight was down to 10.2 pounds (i.e., a 1 pound weight loss). The cat also had mild anisocoria, and now I could palpate bilateral thyroid nodules!
I performed routine blood work (CBC, serum chemistry panel) which was completely normal. Her serum T4 value was also normal at 1.5 µg/dl (reference range, 0.8 - 4.0 µg/dl), and the free T4 by dialysis was normal at 23 nmol/L (reference range, 10-50 nmol/L).
It's amazing how much this cat has deteriorated in just 3 months. How can you explain the cat's thyroid goiter with the normal T4 and free T4 results? Do my results rule out thyroid disease?
My Response:
Both the serum thyroid tests and history rule out hyperthyroidism, but this cat could still have thyroid hyperplasia or neoplasia. The cervical masses you palpate certainly may be thyroid nodules but could also be lymph nodes, parathyroid tumors, or another type of subcutaneous tumor.
I'd start with fine needle aspiration of the cervical masses. Those results will dictate where our workup should go next. If those results are consistent with thyroid tissue, the next step would be to do thyroid scan (scintigraphy) in order to document that the cervical tumors are indeed thyroid in origin and to rule out thyroid carcinoma.
Źródło: endocrinevet.blogspot.com
How do we best diagnose hyperadrenocorticism in dogs? Which is the best diagnostic test? A presumptive diagnosis of should be made from clinical signs, physical examination, routine laboratory tests, and diagnostic imaging findings, but the diagnosis must be confirmed by use of cortisol hormone assays and pituitary-adrenal function tests. For screening tests designed to diagnose Cushing's syndrome, we have three choices:
* ACTH stimulation test
* Low-dose dexamethasone suppression test (LDDST)
* Urinary cortisol:creatinine ratio (UCCR)
Which screening test is best?
Unfortunately, none of the diagnostic tests used in dogs with suspected Cushing's syndrome are totally reliable, and both false-positive and false-negative results are common. Because there are inherent problems with these diagnostic tests, the veterinarian is frequently challenged when attempting to properly interpret the dog’s tests results. It is important to remember, however, that the predictive value of a positive screening test result for Cushing's increases in direct proportion to the number and severity of clinical signs and biochemical changes that develop in this disease. Therefore, one must always remember the importance of the dog’s signalment, history, and physical examination findings when interpreting the diagnostic test results of all pituitary-adrenal function tests.
Who should be tested for hyperadrenocorticism?
Testing for hyperadrenocorticism in a dog should be done because they have one or more clinical signs of the disease. Typically the disease is insidious and slowly-progressive, so most dogs have had clinical signs, such as abdominal enlargement, panting, muscle weakness, thin skin, lethargy, polyphagia, polyuria and polydipsia (PU/PD) for months to even years before the owners recognize a problem and seek veterinary help.
Who should NOT be tested for hyperadrenocorticism?
Testing for Cushing's syndrome is not recommended if the only abnormality is an increased serum alkaline phosphatase (SAP) activity on a serum chemistry panel, and the dog is otherwise apparently healthy. It is difficult enough to interpret endocrine tests in dogs with clinical signs of the disease; if they have no clinical signs, all of the endocrine tests may be difficult to interpret because of false-positive and false-negative results. The first step in workup in these dogs may include an abdominal ultrasound or bile acid testing. One should not screen dogs for hyperadrenocorticism when the dog is sick with clinical signs that would not be related to Cushing's syndrome (e.g., vomiting, anorexia, weight loss). Many non-specific illnesses and other systemic diseases will produce false-positive results with the endocrine tests. Remember, hyperadrenocorticism is only slowly progressive, so hyperadrenocorticism is never an emergency diagnosis. Before diagnostic testing is performed, it is therefore always good to ask oneself: if the test results would indicate hyperadrenocorticism, would I then feel confident to start treating with mitotane (Lysodren®) or trilostane (Vetoryl®) given the clinical picture of the patient? Would treatment help the dog's clinically signs? If either answer is "no," then it is probably best not to screen for hyperadrenocorticism in the first place.
My dog has clinical signs of hyperadrenocorticism and now other nonrelated illness - now can I test?
If the dog has any or all of the clinical signs of hyperadrenocorticism, yes, you should proceed with testing of the pituitary-adrenal axis. However, it is necessary first to ensure that the dog is not being exposed to exogenous glucocorticoids, including topical glucocorticoids on the eyes, ears or skin. First check with the owner to ensure that they are not applying topical glucocorticoids to their own skin - sometimes, dogs may ingest glucocorticoids by licking steroid-containing cream off of the owner's skin. If there is any doubt, ask the owner to bring in all and any medications that dog is receiving (including over the counter preparations) and anything that the owner or owner's family might be using in order to verify that no glucocorticoids are in any of these medications. Next, obtain a routine database (CBC, serum chemistry analysis, and complete urinalysis) before any endocrine testing is undertaken. Finding the expected clinical pathology changes in a dog with suspected Cushing's syndrome helps confirm what the initial history and physical exam suggested. Typical abnormalities in dogs with hyperadrenocorticism include high values for serum alkaline phosphatase, alanine aminotransferase, low to low-normal serum urea nitrogen, and dilute urine specific gravity. On the CBC, we may see a 'stress' leukogram (elevated mature neutrophils and monocytes, decreased lymphocytes and eosinophils), and a hematocrit and RBC count at the high end of normal.
What about now? Now should I use one of the screening tests?
If all the analyses point to hyperadrenocorticism at this stage, test away! In the next blog, I'll be discussing the pros and cons of the ACTH stimulation test for Cushing's syndrome.
Źródło: endocrinevet.blogspot.com










